Katie Lynn (she/her/hers) earned her master’s degree in environmental studies at the College of Charleston (Charleston, SC), focusing on the ways in which climate change, socio-political environments, and human migration impact the distribution of vector-borne disease. She began working at the University of South Carolina as a research associate, coordinating projects and leading pathogen testing for neglected parasitic infections, primarily in pediatric populations, in the US and El Salvador. Katie began pursuing her Ph.D. in Epidemiology at the University of South Carolina in 2019 and is now in her third year in the Laboratory of Vector-Borne and Zoonotic Diseases at the University of South Carolina’s Arnold School of Public Health. Her research interests lie in characterizing neglected tropical diseases (NTDs) and health disparities through a socioecological lens in a global context, and culturally competent intervention strategies for NTDs in the maternal-child health space. Ms. Lynn is currently working as the graduate assistant for the Carter Center’s Trachoma Control Program for the 2021-2022 academic year investigating hyperendemicity in trachoma persistent districts. Katie is also currently working on her dissertation focusing on congenitally transmitted neglected tropical disease and an enhanced pediatric gastrointestinal parasite treatment intervention in El Salvador.
My Introduction to Interdisciplinary/Interprofessional Team Building
I became interested in infectious disease research during my undergraduate studies while taking a microbial ecology class. I always knew I wanted to work with environmental and public health, but this course really piqued my interest in the infectious disease world. While pursuing my master’s degree in environmental sciences, one of my favorite courses was on political ecology and environmental governance, which drove home how power structures, resource distribution, and environmental health are tied to human health and disease. This is where I began thinking of how these factors, which mostly impact vulnerable populations, influenced infectious diseases. Looking at infectious disease through a socioecological lens was the primary focus of my master’s thesis, and is still one of my primary research interests now. Think of it as One Health (the connection between human/animal/environmental health) but with the environment aspect broken down not only into the place we live in, but the social and political structures/spaces in which we live that further influence what resources we have access to (clean water, sanitation, health care), and what behaviors we engage in (washing our hands/going to the doctor).

Because NTDs, in particular, affect predominately the most vulnerable with the fewest resources, I became interested in NTDs and in working with mothers and children who are often most affected by these diseases. To narrow my focus and complete my thesis, I needed a committee of experts in the field and had to pitch my idea to many faculty outside of our department. This was a great exercise in science communication! I was very fortunate to be connected with some outstanding professors at my university that were inquisitive and interested in meshing their combined expertise into a somewhat newer focus area for all of us and our program. In the end, our team was comprised of researchers from human geography, environmental science, public health, and African politics. With (a lot) of help from each individual’s skill set, we were able to create a thesis project that ended up winning a university thesis award and resulted in a peer-reviewed publication.
Lessons Learned
From this experience, I learned a few important lessons that I will continue to carry with me as I pursue my Ph.D. and future career. 1) Communication is key! In order to build strong partnerships, it was essential for me to communicate clearly how the research question filled gaps in the literature, how my research was related to and pertinent to the specific fields of my faculty mentors, and what expertise I lacked where they could contribute. It was also essential that I listened to their expertise and guidance as we collaboratively developed a research plan. 2) Be proactive! To find a team that was interested in the developing project at hand, I had to spend a lot of time sending emails, making phone calls, and attending meetings. 3) Have patience! Building a team did take time and required patience as I searched for the right team members that had both the time and the interest in the project at hand. I also had to be patient with myself as there was a lot I did not know. I had to be open to learning new things and flexible to differing ideas and changes that needed to be made to make the project successful.
Current application of Interdisciplinary/Interprofessional Team Building
Since 2018, I have worked for the Laboratory of Vector-Borne and Zoonotic Diseases at the University of South Carolina, under P.I., Dr. Melissa Nolan. One of our primary areas of research revolves around Chagas disease, a parasitic infection that causes severe cardiac outcomes in one-third of those chronically infected. Individuals become infected primarily when parasite-infected fecal material from the triatomine insect vector enters the body through abrasions in the skin or the mucosa. The disease is also transmitted congenitally in approximately 5% of infected mothers and up to 40% of vertically infected neonates are symptomatic at delivery. However, the rate of congenital transmission is thought to vary considerably between endemic regions. Due to vector control efforts, the global case burden is decreasing every year. As global case counts decline, the proportion of global cases comprised of congenital infection becomes increasingly important, with 22.5% of current incident cases estimated to be congenitally acquired. Congenital Chagas disease has been prioritized for public health action by the World Health Organization and is of particular importance due to the high efficacy of trypanocidal treatment in children <1 year.
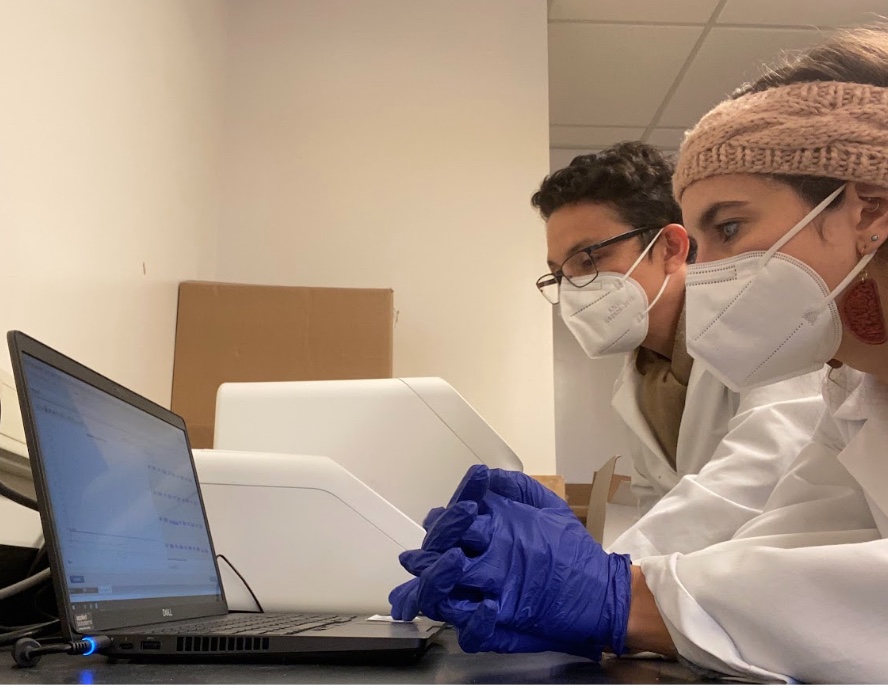
As part of my dissertation work, we sought to implement screening of pregnant women in a high-risk region of El Salvador, where we have previously worked to understand pediatric acute Chagas disease and gastrointestinal parasite co-infection. To begin this project, we had to get approvals from the Ministry of Health and go through a national ethics committee process. We had to assemble a team of physicians and nurses from our prospective hospital study site, along with molecular biologists and laboratory technicians from our long-time partners at the Centro de Investigación y Desarrollo en Salud (CENSALUD), University of El Salvador. The goal of this current project is to understand the prevalence of congenital Chagas disease in this region, the mechanism in which the parasite is able to cross the placental barrier, and concurrently circulating infectious causes of neonatal morbidity. This project builds capacity for prenatal screening in a highly Chagas disease-endemic region. The outcomes of this project will inform prenatal care in this region and clinical screening guidelines for high-risk regions of El Salvador.

